MSU neurologist honored for providing access to patient care during pandemic
October 4, 2021 - Lynn Waldsmith
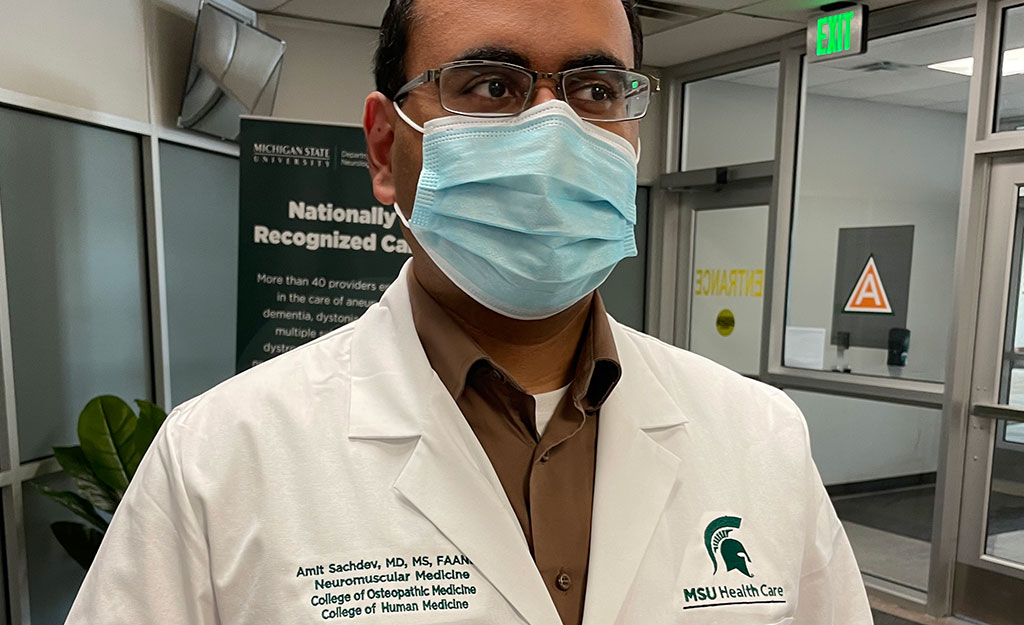
Dr. Amit Sachdev receives Notable Rising Star in Health Care Leadership Award from Crain’s Detroit Business for his efforts to ensure that patients continue to receive care during the public health crisis.
Amit Sachdev, MD, had a very bad feeling.
It was the first week of March 2020; the Trump administration had not yet declared the coronavirus pandemic a national emergency and the WHO had not yet even declared the spread of COVID-19 a pandemic. Nationally, many health professionals were saying that the flu posed a greater threat than the coronavirus.
But Dr. Sachdev’s mind was a step ahead. He was ordering supplies. He knew that Michigan State University’s (MSU) Department of Neurology and Ophthalmology had to act fast to keep seeing hundreds of patients per week.
"I’m old enough to remember what happened to Toronto with SARS."Amit Sachdev, MD
“I’m old enough to remember what happened to Toronto with SARS,” said Dr. Sachdev, recalling that city’s SARS outbreak in 2003. “That one city nearly shutdown. Here we had (COVID-19) popping up around the globe. I never imagined that we would have to make these modifications for such a long time.”
The modifications Dr. Sachdev and his colleagues set in motion may seem commonplace now — mask wearing, social distancing, patients waiting in their cars, video and telephone office visits. But the introduction of telemedicine for patients who seek neurologic care from MSU Health Care was largely made possible through Dr. Sachdev’s efforts to take quick action.
Dr. Sachdev, an expert in rare nerve and muscle diseases, is an associate chief medical officer at MSU Health Care and medical director for MSU Health Care Neurology and Ophthalmology.
“What strikes me the most is he has an engineering background that, once the pandemic hit, was really a key asset in dealing with a very complicated situation,” said Dr. Anthony Avellino, who nominated him for the award. As MSU’s assistant vice president for health sciences and MSU Health Care chief clinical and medical officer, Dr. Avellino oversees and promotes quality and safety initiatives designed to improve clinical effectiveness.
“(Dr. Sachdev’s) ability to integrate multiple pieces of the puzzle was instrumental in developing and creating clinical processes and flow and safety protocols that resulted in a highly successful telemedicine platform. He’s passionate about what he does and in health care we need more passionate people like him.”
Dr. Sachdev says he is humbled by the award and that “launching telemedicine for neurology was a team effort.” Yet, he agrees, his engineering background helped him to study and overcome the intricacies of delivering patient care during the public health crisis.
“Being an engineer and a neurologist has helped me visualize health care systems,” he explained. “Health care systems are very complicated, but they’re also predictable. It begins with ‘A’ goes with ‘B’ and just multiplies exponentially from there, like dominos. Being able to understand that complexity has served me well.”
“What strikes me the most is he has an engineering background that, once the pandemic hit, was really a key asset in dealing with a very complicated situation"
Anthony Avellino, MD
Providing access to quality health care was his greatest worry when COVID-19 began to spread in the U.S.
“We had no infrastructure for telehealth at that time. None,” said Dr. Sachdev. “Finances was the second biggest concern. If you can’t give patients access to care, then you have failed at your primary mission. And by the way, if we fail at delivering care then we can’t keep our lights on.”
When government-led lockdowns began in mid-March of 2020, health care was being delivered face to face. By early April 2020, 97 percent of Neurology patients were scheduled for video or telephone office visits. According to Dr. Sachdev, the department’s total number of patient encounters declined about 30 percent, but not 80 to 90 percent as some health care systems experienced. While the IT experts at MSU Health Care focused on the nuts and bolts of conducting virtual office visits, each department was tasked with delivering telemedicine according to its own needs. Dr. Sachdev credits much of the department’s success to sheer “bull headedness”.
“We hit the phones and called patients,” he said. “The vast majority of them just assumed we would be closed. The reason we were able to execute so many encounters is we had the will to make it work. We just made it work.”
Due to national interest, he and other senior leaders of MSU Health Care gave a presentation to members of The Patient Access Collaborative in June of 2020 to explain how various departments at MSU successfully rolled out telehealth at the onset of the pandemic.
While more patients are now being treated in person again, Dr. Sachdev is confident telemedicine is here to stay. How it is paid for in the future will be the challenge. Once the pandemic is over, continued delivery of telehealth will depend changes in federal law.
“We have to maintain access to telemedicine,” Dr. Sachdev said. “There’s so much care that can be delivered virtually. It shouldn’t be that you have to take a day off work to be seen by a provider, or take a kid out of school, or drive, in some cases, hundreds of miles. It just doesn’t make sense.” Sachdev led the writing of MSU Health Care’s appeal to lawmakers to make the appropriate changes to maintain access.
As for what is next? “Inequality” says Dr. Sachdev, “we must act now to write the ending to the COVID19 chapter.". The pandemic has left millions with post-COVID neurologic disease and opioid deaths have increased substantially. "Every opioid death begins with physical or emotional pain. Physical and emotional pain is treated with medications that work on the brain. Neurology has to step in, we are the brain people. There are not enough neurologists, so we must work in teams with nurse practitioners, social workers and physicians assistants.”